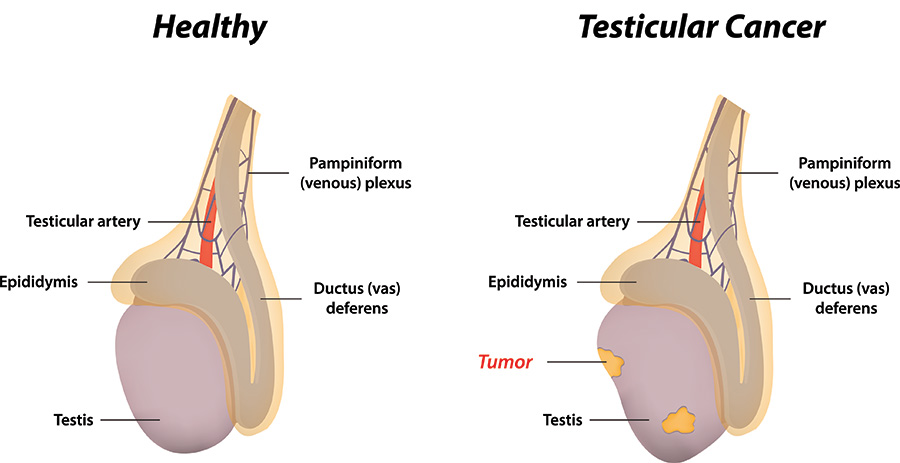
Testicular cancer is highly treatable, especially when detected early. Treatment options vary based on the cancer stage, diagnostic test results, and the patient’s overall health and preferences. Common approaches include surgery (orchiectomy), radiation therapy, and chemotherapy. In some cases, active surveillance is recommended post-surgery. Each treatment plan is tailored to ensure the best outcomes with minimal side effects. Consulting a specialized oncologist helps determine the most effective strategy. Early diagnosis and timely treatment significantly improve the survival rate. If you or a loved one is facing testicular cancer, exploring personalized treatment options with a healthcare professional is essential.
1. Surveillance
- Surveillance involves close monitoring without immediate treatment.
- Regular physical exams, tumor marker tests, and imaging studies are used to watch for any signs of cancer progression.
- It is often recommended for Stage 0 cancers or after surgery in certain cases.
2. Surgery
Surgery is a primary treatment for testicular cancer, with different types based on cancer type and stage. Before undergoing surgery, it’s important to discuss fertility concerns, as some procedures may affect semen quality and the ability to have children.
1. Orchidectomy (Radical Inguinal Orchiectomy)
- This is the most common surgery for both early and advanced stages.
- A cut is made in the groin to remove the affected testis and spermatic cord.
- The removed tissue is sent for biopsy (histopathological analysis) to confirm the diagnosis.
Post-Surgery:
- Future treatment decisions depend on biopsy results, tumor markers, and imaging.
- Regular follow-ups are essential to check for recurrence.
2. Testis-Sparing Surgery (TSS)
- In TSS, only the tumor is removed, and the rest of the testicle is preserved.
- Suitable only for very small masses and negative tumor markers.
- Typically used for benign tumors, not recommended if the cancer is malignant or if the other testicle is healthy.
Post-Surgery:
- Regular surveillance is essential.
- May affect fertility despite being less invasive.
3. Retroperitoneal Lymph Node Dissection (RPLND)
- A complex surgery used for Stage 1 non-seminomatous germ cell tumors.
- Involves removing lymph nodes from the abdomen to prevent cancer spread.
Post-Surgery:
- Surveillance and possibly chemotherapy may follow, depending on cancer type and spread.
- This surgery helps reduce the risk of recurrence but requires careful monitoring.
3. Radiation Therapy
- Used primarily for seminomas, which are sensitive to radiation.
- Targets cancer cells in the testicle or nearby lymph nodes.
- Not effective for non-seminomas, as they typically don’t respond to radiation.
- Radiation is also used when cancer has spread to other parts of the body.
4. Chemotherapy
- Involves cancer-killing drugs delivered orally or through an IV, allowing them to reach cancer cells throughout the body.
- Often used:
- When cancer has spread.
- If tumor markers rise after surgery.
- To reduce the risk of recurrence.
Chemo is typically a systemic treatment and may be used alone or combined with other therapies depending on the situation